Despite years of scholarly research and evidence supporting the effectiveness of neurofeedback, many people still may have questions about it: how it works, its efficacy, and whether it’s worth exploring as an alternative to traditional treatment.
To help answer your questions, Narbis has put together a list of FAQs and general information about neurofeedback, as well as links to published articles and peer-reviewed research on the subject.
What is neurofeedback?
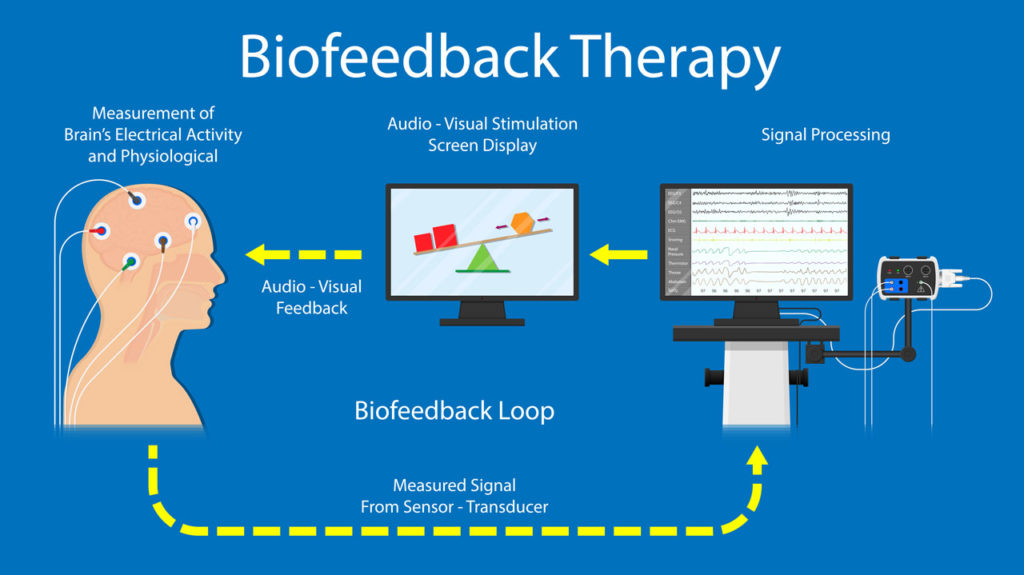
Neurofeedback, a form of biofeedback, is a non-invasive, non-drug way to change the way your brain functions. By monitoring your brainwave activity using electrodes (electroencephalography, or EEG), neurofeedback gives you personalized feedback about how your brain works, rewarding healthy brainwave activity over unhealthy activity, leading to a reduction in unwanted symptoms and behavior.
Neurofeedback has applications for a wide range of conditions including attention disorders like ADHD, and mental health issues such as depression, anxiety, and PTSD. It can also be used to enhance normal functioning, improve overall mental performance, and restore calm and focus to a frazzled mind.
How does neurofeedback work?
According to Harvard-trained neurobiologist Tedi Asher, an important premise of neurofeedback training is that our brains have the ability to change the way they function. Research over the last several decades indicates that our brains are, in fact, malleable. The question, then, is how to influence brain function to stimulate this change.
The trick to getting our brains to act in desirable ways is to leverage the behavior-changing power of operant conditioning, Asher explains in Harvard’s ‘Science in the News’. Akin to how dogs learn to sit when given a treat, humans learn in very similar ways, including teaching ourselves to promote healthier brain activity.
- In neurofeedback training, enhancing brain functioning is accomplished by pairing information about one’s brain activity with desirable or undesirable outcomes.
- When we generate desirable brain activity, we are rewarded; when we generate unwanted activity, we aren’t.
- Repeated exposure to such gains and losses can bring about long-lasting changes in brain activity.
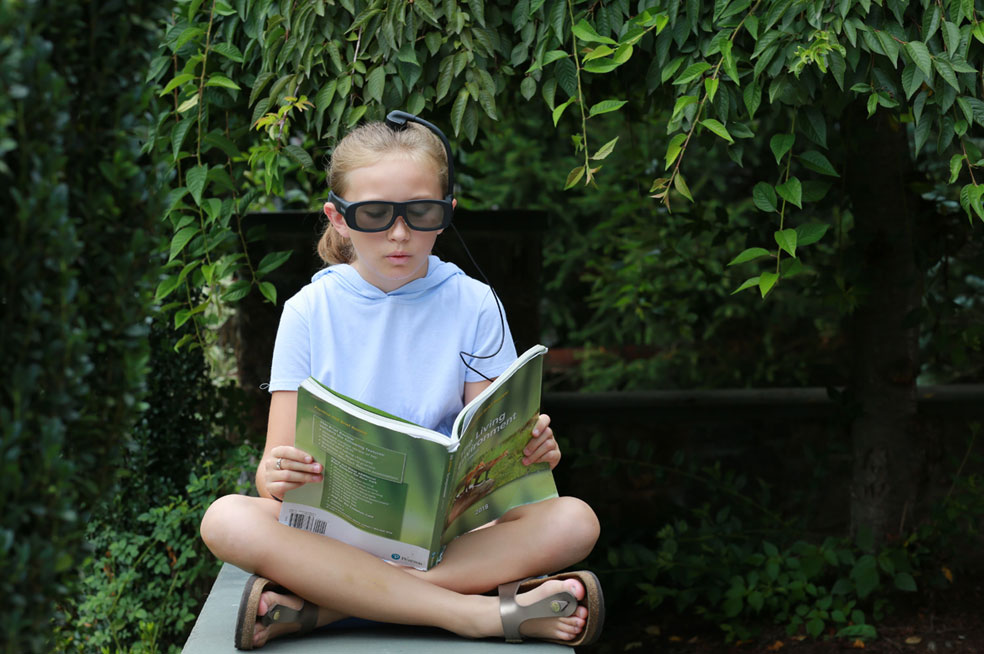
For example, Narbis smart glasses provide instant feedback to recognize when you are distracted, giving you the cue to get back on task. Sensors in the Narbis glasses and a NASA-patented algorithm track your brain’s state: whether you’re distracted, relaxed, or focused. When your attention drifts, the glasses change tint and when you focus, they clear. The glasses help your brain identify these positive behaviors which encourages you to shift into a more focused, attentive state.
What scientific evidence exists to support neurofeedback treatment?
- Neurofeedback has a 75+ year history of scientific research documenting operant conditioning with EEG in cats (Wyrwicka & Sterman, 1968), primates (Schafer & Moore, 2011), and people (Jasper & Shagass, 1941).
- Neurofeedback also has a 50+ year clinical use history as a trusted tool for clinicians treating ADHD, as well as other neurological disorders including insomnia, PTSD, anxiety, depression, traumatic brain injury, and dementia.
How can neurofeedback help treat attention disorders?
Neurofeedback is becoming increasingly popular as a way to treat people struggling with neurological or psychiatric disorders, such as children diagnosed with attention deficit hyperactivity disorder (ADHD).
Several randomized controlled trials have been conducted comparing neurofeedback to non-pharmacological treatments, and even more studies have compared neurofeedback to stimulant medication in treating ADHD’s core symptoms. The results are conclusive:
A focused brain acts differently from an unfocused one, and neurofeedback training can help children induce a brain state that’s characteristic of showing focus.
What follows are brief summaries of the findings from these aforementioned randomized controlled trials comparing neurofeedback to other non-pharmacological treatments for ADHD. Some findings from these studies:
Neurofeedback and non-pharmacological ADHD treatment research studies:
- In double-blinded reversal design studies, Lubar and Shouse (1976; 1979) demonstrated both the functional relationship between the sensory motor rhythm and ADHD behaviors and that through real-time sensory motor rhythm feedback paired with operant conditioning, ADHD children could learn to self-regulate sensory motor rhythm, and thus control their ADHD behaviors.
- Neurofeedback was superior to cognitive training programs in four randomized control trials with a combined “n” of 270 subjects (Drechsler et al., 2007; Holtmann et al., 2009; Gevensleben et al., 2010; Steiner et al., 2014). In one study (n=29), it was equivalent to self-management training, an evidence-based ADHD treatment that is mandated for insurance coverage in Germany (Christiansen et al.,2014).
- Two randomized controlled trials compared electromyographic (EMG) biofeedback to neurofeedback to control for both non-specific effects as well as the effects of self-regulation training (Bakhshayesh et al., 2011; Strehl et al., 2017). Both of these studies found that subjects learned to self-modulate the targeted behavior (either EMG or EEG) with neurofeedback, demonstrating significant superiority over EMG in reducing ADHD symptoms.
- The meta-analysis of five randomized controlled trials of neurofeedback in children with ADHD, (Jean-Arthur Micoulaud-Franchi, 2014) highlights improvement in the inattention dimension of ADHD symptoms.
- A systematic review (Sampedro Baena, 2021) was carried out of nine articles to analyze the effects of neurofeedback interventions in children with ADHD. The review found that NF improved behavior, allowed greater control of impulsivity, and increased sustained attention. In addition, it improved motor control, bimanual coordination and was associated with a reduction in theta waves.
- A randomized controlled experiment was carried out over six months to evaluate sustained attention training improvements using neurofeedback or cognitive training for 7- to 11- year-olds with ADHD, (Steiner, 2014). During the study, 104 children were randomly assigned to receive neurofeedback, or a control condition and were evaluated six months post intervention. A three-point growth model assessed change over time across the conditions. It found that Neurofeedback participants made more prompt and greater improvements in ADHD symptoms, which were sustained at the six-month follow-up, than those in cognitive training and the control group.
Neurofeedback and stimulant medication for the treatment of ADHD research studies:
The following summarizes the findings from eight head-to-head comparisons of neurofeedback to stimulant medication for the treatment of ADHD. These studies found that neurofeedback treated ADHD core symptoms just as well as stimulant medication:
- Neurofeedback for the treatment of children and adolescents with ADHD: a randomized and controlled clinical trial using parental reports Duric et al., 2012; BMC Psychiatry
- Treatment of ADHD: comparison of EEG-biofeedback and methylphenidate Flisiak- Antonijczuk et al., 2015; Archives of Psychiatry and Psychotherapy
- Neurofeedback Treatment for Attention-Deficit/Hyperactivity Disorder in Children: A Comparison With Methylphenidate Fuchs et al., 2003; Applied Psychophysiology and Biofeedback
- An RCT into the effects of neurofeedback on neurocognitive functioning compared to stimulant medication and physical activity in children with ADHD Gelade et al., 2017; European Child & Adolescent Psychiatry
- Neurofeedback and Standard Pharmacological Intervention in ADHD: A Randomized Controlled Trial With Six-Month Follow-Up Meisel et al., 2013; Biological Psychology
- Neurofeedback, pharmacological treatment and behavioral therapy in hyperactivity: Multilevel analysis of treatment effects on electroencephalography Moreno-Garcia et al., 2017; International Journal of Clinical and Health Psychology
- The Effectiveness of Neurofeedback and Stimulant Drugs in Treating AD/HD: Part I. Review of Methodological Issues Rossiter, 2004; Applied Psychophysiology and Biofeedback
- A comparison of EEG biofeedback and psychostimulants in treating attention deficit/hyperactivity disorders Rossiter and La Vaque, 1995; Journal of Neurotherapy
These eight studies comprised 581 subjects. In only one head-to-head comparison (n=32) were stimulants found superior to neurofeedback (Ogrim and Hestad, 2013). These comparative effectiveness studies provide strong evidence that neurofeedback is an evidence-based treatment option for ADHD.
The largest and most rigorous of these studies (Gelade et al., 2017) did a follow-up study and analysis (Janssen et al., 2016) and found that both neurofeedback and stimulant medication treatments resulted in “comparable reductions in theta power from pre- to post-intervention.” suggesting a similar change/response mechanism from these two treatments. (To learn more about the differences among alpha, beta, and theta brainwaves, check out this article in Scientific American).
One randomized control trial that found stimulant medication combined with neurofeedback showed superior results at the end of treatment and six-month follow-up to stimulant medication combined with attention training.
In two of the most compelling studies (Duric et al., 2012 and Gelade et al., 2016) neurofeedback was found to produce a significant improvement in the core symptoms of ADHD and was found to be equivalent or superior to the effects produced by methylphenidate, commonly known as Ritalin.
Neurofeedback studies demonstrate that learning is associated with improvements on a wide variety of ADHD outcome measures of interest, and both are sustained at follow-up (e.g., Strehl et al., 2006; Leins et al., 2007; Gelade et al., 2017) even up to two years later (Gani, Birbaumer & Strehl, 2008). These findings show that one’s ability to self-modulate using neurofeedback is well beyond any outcomes seen using placebo.
Additionally, this review paper, “Neurofeedback: A Comprehensive Review on System Design, Methodology and Clinical Applications,” catalogs how neurofeedback is used and for what, with links to commonly-cited studies and scientific literature on the topic. The authors provide clinical and technical information about the following issues:
- Various neurofeedback treatment protocols i.e. alpha, beta, alpha/theta, delta, gamma, and theta;
- Different EEG electrode placements i.e. standard recording channels in the frontal, temporal, central, and occipital lobes;
- Electrode montages (unipolar, bipolar);
- Types of neurofeedback i.e. frequency, power, slow cortical potential, functional magnetic resonance imaging, and so on;
- Clinical applications of neurofeedback i.e. treatment of attention deficit hyperactivity disorder (ADHD), anxiety, depression, epilepsy, insomnia, drug addiction, schizophrenia, learning disabilities, dyslexia and dyscalculia, autistic spectrum disorders and so on as well as other applications such as pain management, and the improvement of musical and athletic performance; and
- Neurofeedback software
In the meta-analysis of a series of 10 randomized controlled studies conducted over 12 months assessing the sustainability of neurofeedback effects among children with ADHD (Van Doran, 2018), the results of NF treatment follow-up suggest that there are sustained symptom reductions over time in comparison with non-active control conditions. The improvements seen during the study were comparable to children using the drug methylphenidate to treat ADHD.
“As such, NF can be considered a non-pharmacological treatment option for ADHD with evidence of treatment effects that are sustained when treatment is completed and withdrawn,” the study says.
What other questions do you have about neurofeedback?

We want to hear from you. What else do you want to know about neurofeedback? Drop us a line at info@narbis.com and we’ll do our best to answer you. We might even add your question to this list! We’ll continue to keep this page updated so keep checking back, or you can also sign up for our newsletter HERE.